Material imaging study of 3D printing materials for diagnostic radiology phantom development
DOI:
https://doi.org/10.15392/2319-0612.2024.2556Palabras clave:
3D printing, Fused Filament Fabrication, phantom, Signal-to-Noise Ratio, Contrast-to-Noise RatioResumen
The 3D printing techniques have found applications across diverse fields, significantly enhancing design and manufacturing processes. The impact of this growth is particularly notable in radiology, where 3D printing has been applied to developing quality control tools and advancing dosimetry techniques. 3D printing has the advantage of having a wide variety of plastic materials which can be used in the manufacturing process; there is a scarcity of work developed to evaluate the attenuation of the x-ray beam of the materials used in printing 3D models for phantom development. This paper aims to show our results on the imaging characteristics investigation of 15 3D printable materials. 3D objects were printed as cubes of 20 x 20 x 20 mm3 with a 100% infill and 45°/45° rectilinear structural pattern, and images acquired in a DR X-ray unit were analyzed with ImageJ software. Imaging pixel values, Signal-to-Noise Ratio – SNR and Contrast-to-Noise Ratio – CNR were evaluated and compared between the 3D-printed cubes and a standard chest phantom. When comparing the SNR for plastic materials and chest structures, significant differences were found. Similar results were found for the CNR. The differences were noted for both plastic materials, Tungsten and Bismuth, that demonstrated statistically significant values of SNR compared to the lung (p < 0.0001) and right rib (p < 0.0001). Tungsten and Bismuth filaments were found to have the potential to represent the SNR for intermediary and high-density structures. Scapula was the only anatomical structure with no statistically significant difference of the CNR for SILK (p ≥ 0.074), ABS (p ≥ 0.086), PVA (p ≥ 0.917) and ABSpremium (p ≥ 0.955). The study of potential radiological 3D printing materials for diagnostic radiology phantom development revealed important imaging characteristics for the plastic materials using the Fused Filament Fabrication technique.
Descargas
Referencias
CRAMER, J.; QUIGLEY, E.; HUTCHINS, T.; , SHAH, L. Educational Material for 3D Visualization of Spine Procedures: Methods for Creation and Dissemination J. Digit. Imaging, v.30, n.3,p.296-300, 2017. DOI: https://doi.org/10.1007/s10278-017-9950-0
KAMOMAE. T.;, SHIMIZU, H.; NAKAYA, T.; OKUDAIRA,K.;AOYAMA, T.; OGUCHI, H.; KOMORI, M.; KAWAMURA, M.; OHTAKARA,K.; MONZEN, H.; ITOH, Y.; NAGANAWA,S.; Three-dimensional printer-generated patient-specific phantom for artificial in vivo dosimetry in radiotherapy quality assurance Phys. Medica, v. 44 , p. 205-211, 2017 DOI: https://doi.org/10.1016/j.ejmp.2017.10.005
SCULPTEO. The State of 3D Printing Report 2018 Disponível em: https://www.sculpteo.com/en/ebooks/state-of-3d-printing-report-2018/. Acesso em: 27 ago. 2024
SHIN, J.; SANDHU, R.. S.; SHIH, G.; Imaging Properties of 3D Printed Materials: Multi-Energy CT of Filament Polymers J. Digit. Imaging, v.30,n.5, p.572–5, 2017 DOI: https://doi.org/10.1007/s10278-017-9954-9
YANG, L.; GROTTKAU, B.; HE, Z.; YE, C. Three dimensional printing technology and materials for treatment of elbow fractures Int. Orthop., v.41,p. 2381–2387, 2017. DOI: https://doi.org/10.1007/s00264-017-3627-7
FAROOQI, K. M.; SAEED, O.; ZAIDI, A.; SANZ, J.; NIELSEN, J. C.; HSU, D. T.; JORDE, U. P. 3D Printing to Guide Ventricular Assist Device Placement in Adults With Congenital Heart Disease and Heart Failure. JACC Hear. v.4,n.4, p.301-11, 2016 DOI: https://doi.org/10.1016/j.jchf.2016.01.012
SAVI, M.; ANDRADE, M. A. B.; POTIENS, M. P. A. Commercial filament testing for use in 3D printed phantoms, Radiat. Phys. Chem., v. 174, p, 108906, 2020 DOI: https://doi.org/10.1016/j.radphyschem.2020.108906
SAVI, M.; ANDRADE, M. A. B.; VILLANI, D., JUNIOR, O. R.; POTIENS, M. D.A. P. A. Development of radiopaque FFF filaments for bone and teeth representation in 3D printed radiological objects, Brazilian J. Radiat. Sci. v.10,n.1,p.01-22,2022. DOI: https://doi.org/10.15392/bjrs.v10i1.1739
KAPETANAKIS, I.; FOUNTOS, G.; MICHAIL, C.; VALAIS, I.; KALYVAS, N.; 3D printing X-Ray Quality Control Phantoms. A Low Contrast Paradigm, Journal of Physics: Conference Series,v.931,p. 012026,2017 DOI: https://doi.org/10.1088/1742-6596/931/1/012026
OLIVEIRA, M.; BARROS, J.C.; UBEDA, C. Development of a 3D printed quality control tool for evaluation of x-ray beam alignment and collimation, Phys. Medica, v. 65, p.29-32, 2019. DOI: https://doi.org/10.1016/j.ejmp.2019.07.026
PAXTON. N.; SMOLAN, W.; BÖCK, T.; MELCHELS, F.; GROLL, J.; JUNGST, T.; Proposal to assess printability of bioinks for extrusion-based bioprinting and evaluation of rheological properties governing bioprintability Biofabrication v.9,n.4,p.044107, 2017 DOI: https://doi.org/10.1088/1758-5090/aa8dd8
OGDEN,K. M.; MORABITO, K. E.; DEPEW, P. K.; 3D printed testing aids for radiographic quality control J. Appl. Clin. Med. Phys. v.20,n.5,p. 127–34,2019 DOI: https://doi.org/10.1002/acm2.12574
NOONOO. J, B.; SOSU, E.; HASFORD, F.; Three-dimensional image quality test phantom for planar X-ray imaging. S. Afr. J. Sci.v.119,n.7/8, p.1-7,2023 DOI: https://doi.org/10.17159/sajs.2023/14269
MADAMESILA, J.; MCGEACHY, P.; VILLARREAL, B.J. E.; KHAN, R. Characterizing 3D printing in the fabrication of variable density phantoms for quality assurance of radiotherapy, Phys. Medica, v.32,n1,p.242-247, 2016 DOI: https://doi.org/10.1016/j.ejmp.2015.09.013
GROENEWALD, A.; GROENEWALD, W. A. Development of a universal medical X-ray imaging phantom prototype J. Appl. Clin. Med. Phys. v.17,n.6,p356-365,2016. DOI: https://doi.org/10.1120/jacmp.v17i6.6356
SCHOPPHOVEN, S.; CAVAEL, P.; BOCK, K.; FIEBICH, M.; MÄDER, U. Breast phantoms for 2D digital mammography with realistic anatomical structures and attenuation characteristics based on clinical images using 3D printing Phys. Med. Biol.v. 64,n.21,p.215005,2019 DOI: https://doi.org/10.1088/1361-6560/ab3f6a
HE, Y.; LIU, Y.; DYER, B. A.; BOONE, J. M.; LIU, S.; CHEN, T.; ZHENG, F.; ZHU, Y.; SUN, Y.; RONG, Y.; QIU, J.;3D-printed breast phantom for multi-purpose and multi-modality imaging Quant. Imaging Med. Surg. v.9,n.1,p.63-74 ,634–74,2019. DOI: https://doi.org/10.21037/qims.2019.01.05
OLIVEIRA, M.; SAVI, M.; ANDRADE, M.; VILLANI, D.; POTIENS, M. P. A.; STUANI, H; UBEDA, C.; MDLETSHE, S.; Attenuation properties of common 3D printed FFF plastics for mammographic applications Brazilian J. Radiat. Sci.,v. 10.n.1,p.01-17,2022 DOI: https://doi.org/10.15392/bjrs.v10i1.1732
LEE, M. Y.; HAN, B.; JENKINS, C.; XING, L.; SUH, T. S.; A depth-sensing technique on 3D-printed compensator for total body irradiation patient measurement and treatment planning Med. Phys. v.43,n.11,p.6137,2016 DOI: https://doi.org/10.1118/1.4964452
JAVAN, R.; BANSAL, M.; TANGESTANIPOOR, A. A prototype hybrid gypsum-based 3-dimensional printed training model for computed tomography-guided spinal pain management J. Comput. Assist. Tomogr.v.40,n.4,p.626-631,2016 DOI: https://doi.org/10.1097/RCT.0000000000000415
KIM, M. J.; LEE, S. R.; LEE, M. Y.; SOHN, J. W.; YUN, H. G.; CHOI, J. Y.; JEON, S. W.; SUH, T. S. Characterization of 3D printing techniques: Toward patient specific quality assurance spine-shaped phantom for stereotactic body radiation therapy PLoS One, v.12,n.5,p.e0176227,2017 DOI: https://doi.org/10.1371/journal.pone.0176227
SILBERSTEIN, J. ; SUN, Z. Advances and Applications of Three-Dimensional-Printed Patient-Specific Chest Phantoms in Radiology: A Systematic Review Appl. Sci. v.. 14, p. 5467 14 5467, 2024 DOI: https://doi.org/10.3390/app14135467
Rasband W. ImageJ. Bethesda, Maryland, USA: U.S. National Institutes of Health; 1997e2012. Disponivél em:: http://imagej.nih.gov/ij/.
HUDA, W.; ABRAHAMS, R. B. Radiographic techniques, contrast, and noise in x-ray imaging. Am. J. Roentgenol. v.204,n.2,p. W126–31,2015 DOI: https://doi.org/10.2214/AJR.14.13116
BRODER, J. Imaging the Chest: The Chest Radiograph. In Diagnostic Imaging for the Emergency Physician, Expert Consult - Online and Print, p.185–296, 2011. DOI: https://doi.org/10.1016/B978-1-4160-6113-7.10005-5
DUKOV, N.; BLIZNAKOVA, K.; OKKALIDIS, N.; TENEVA, T.; ENCHEVA, E.; BLIZNAKOV, Z.; Thermoplastic 3D printing technology using a single filament for producing realistic patient-derived breast models, Phys. Med. Biol. v.67,n.4,p.045008,2022 DOI: https://doi.org/10.1088/1361-6560/ac4c30
GEAR, J. I.; LONG, C.; RUSHFORTH, D.; CHITTENDEN, S. J.; CUMMINGS, C.; FLUX, G. D. Development of patient-specific molecular imaging phantoms using a 3D printer Med. Phys. v. 41,n.8,p.082502,2014. DOI: https://doi.org/10.1118/1.4887854
ZHANG, F.; ZHANG, H.; ZHAO, H.; HE, Z.; SHI, .; HE, Y.; JU, N.;RONG, Y.; QIU, J. Design and fabrication of a personalized anthropomorphic phantom using 3D printing and tissue equivalent materials, Quant. Imaging Med. Surg. v.9,n.1,p.94-100,2019 DOI: https://doi.org/10.21037/qims.2018.08.01
ANWARI, V.; LAI, A.; URSANI, A.; REGO, K.; KARASFI, B.; SAJJA, S.; PAUL, N. 3D printed CT-based abdominal structure mannequin for enabling research. 3D Print. Med.v.6,n.1,p.1-12 ,2020 DOI: https://doi.org/10.1186/s41205-020-0056-9
PULLEN, M. W.; POOLEY, R. A.; KOFLER, J. M.;VALERO-MORENO, F.; RAMOS-FRESNEDO, A.; DOMINGO, R. A.; PEREZ-VEGA, C.; FOX, W. C.; SANDHU, S. J. S. QUINONES-HINOJOSA, A.; BUCHANAN, I. A. A radiographic analysis of common 3D print materials and assessment of their fidelity within vertebral models Ann. 3D Print. Med.v.8,p.1-7,2022 DOI: https://doi.org/10.1016/j.stlm.2022.100080
HUDA, W.; BRAD, A.R. X-ray-based medical imaging and resolution Am. J. Roentgenol. v.204,n.4,p. W393–397,2015 DOI: https://doi.org/10.2214/AJR.14.13126
ZHAO, Y.; MORAN, K.; YEWONDWOSSEN, M.; ALLAN, J. CLARKE, S.; RAJARAMAN, M.; WILKE, D.; JOSEPH, P.; ROBAR, J. L. Clinical applications of 3-dimensional printing in radiation therapy Med. Dosim. v.42,n.2,p. 150–155,2017 DOI: https://doi.org/10.1016/j.meddos.2017.03.001
CEH, J.; YOUD, T.; MASTROVICH, Z.; PETERSON, C.; KHAN, S.; SASSER, T. A.; SANDER, I. M.; DONEY, J.; TURNER, C.; LEEVY, W. M. Bismuth Infusion of ABS Enables Additive Manufacturing of Complex Radiological Phantoms and Shielding Equipment. Sensors (Basel).v. 17,n.3,p.459,2017 DOI: https://doi.org/10.3390/s17030459
JUNG, J.; SONG, S. Y.; YOON, S. M.; KWAK, J.; YOON, K.; CHOI, W.; JEONG, S. Y.; CHOI, E. K.; CHO, B. Verification of accuracy of CyberKnife tumor-tracking radiation therapy using patient-specific lung phantoms Int. J. Radiat. Oncol. Biol. Phys.v. 92,n.4,p.745-753,2015 DOI: https://doi.org/10.1016/j.ijrobp.2015.02.055
PALLOTTA, S.; CALUSI, S.; FOGGI, L.; LISCI, R.; MASI, L.; MARRAZZO, L. TALAMONTI, C.; LIVI, L.; SIMONTACCHI, G.ADAM: A breathing phantom for lung SBRT quality assurance Phys. Medica,v.49,p.147-155,2018 DOI: https://doi.org/10.1016/j.ejmp.2017.07.004
LARSSON, J.; LIAO, P.; LUNDIN, P.; KRITE, S.E., SWARTLING, J.; LEWANDER, X. M.; BOOD, J.; ANDERSSON-ENGELS, S. Development of a 3-dimensional tissue lung phantom of a preterm infant for optical measurements of oxygen—Laser-detector position considerations, J. Biophotonics,v.11,n.3,p.1-8,2017 DOI: https://doi.org/10.1002/jbio.201700097
HAZELAAR, C.; VAN EIJNATTEN. M.; DAHELE, M.; WOLFF, J.; FOROUZANFAR, T.; SLOTMAN, B.; VERBAKEL, W. F. A. R. Using 3D printing techniques to create an anthropomorphic thorax phantom for medical imaging purposes Med. Phys. v.45,n.1,p.92-100,2018. DOI: https://doi.org/10.1002/mp.12644
KAIRN, T.; CROWE, S. B.; MARKWELL, T. Use of 3D printed materials as tissue-equivalent phantoms In: Jaffray, D. (eds) World Congress on Medical Physics and Biomedical Engineering, Toronto, Canada. IFMBE Proceedings,v.51,p.728-729,2015 DOI: https://doi.org/10.1007/978-3-319-19387-8_179
Descargas
Publicado
Número
Sección
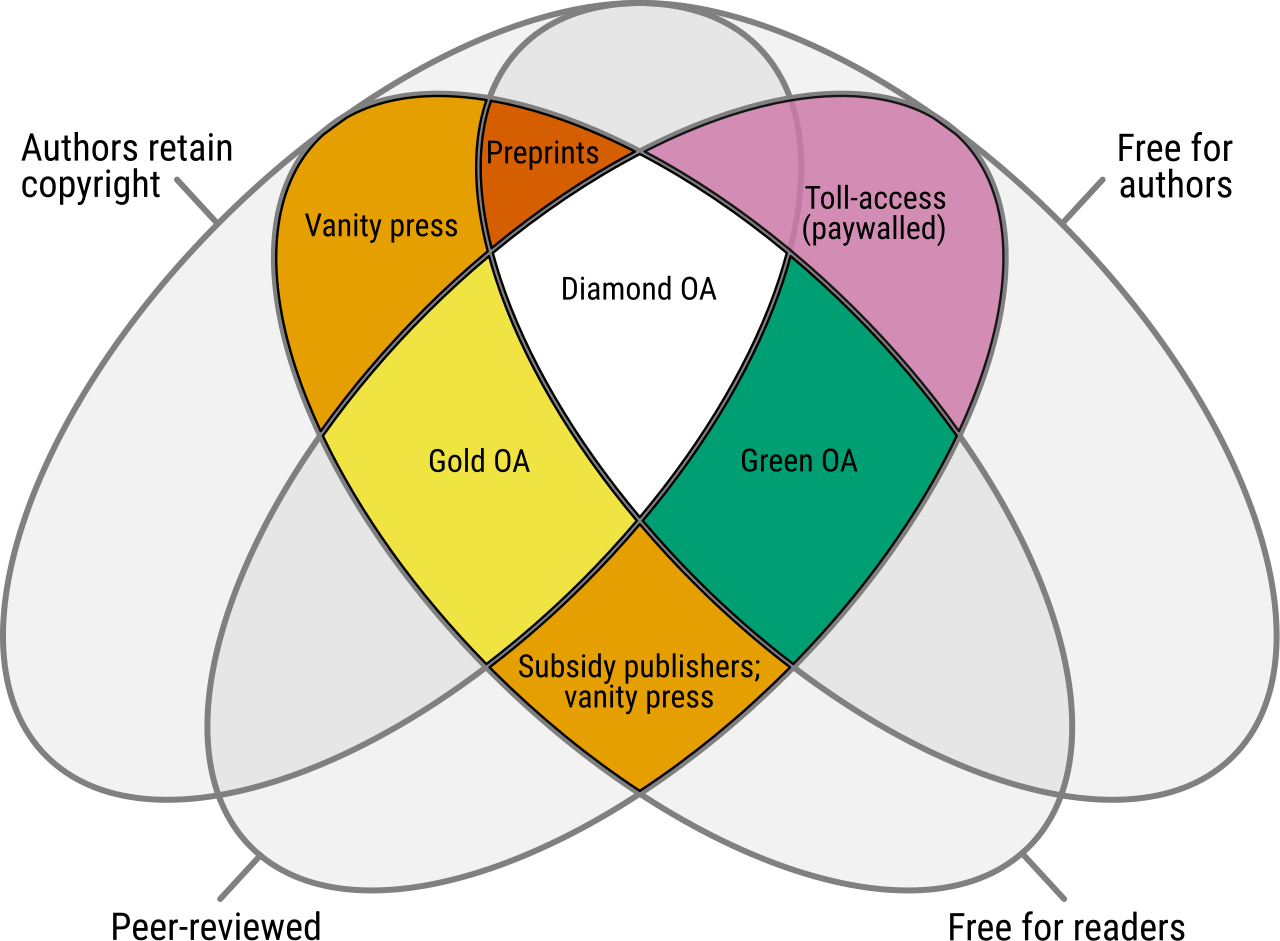
Licencia
Derechos de autor 2024 Brazilian Journal of Radiation Sciences (BJRS)

Esta obra está bajo una licencia internacional Creative Commons Atribución 4.0.
Licencia: los artículos de BJRS tienen una licencia internacional Creative Commons Attribution 4.0, que permite el uso, el intercambio, la adaptación, la distribución y la reproducción en cualquier medio o formato, siempre que se otorgue el crédito correspondiente al autor o autores originales y a la fuente, proporcione un enlace a la licencia Creative Commons e indique si se realizaron cambios. Las imágenes u otros materiales de terceros en el artículo están incluidos en la licencia Creative Commons del artículo, a menos que se indique lo contrario en una línea de crédito al material. Si el material no está incluido en la licencia Creative Commons del artículo y su uso previsto no está permitido por la regulación legal o excede el uso permitido, el autor deberá obtener el permiso directamente del titular de los derechos de autor. Para ver una copia de esta licencia, visite http://creativecommons.org/licenses/by/4.0/